BEBCRF Support Group Meeting – Toronto, Spring 2018
BEBCRF and Cranial Dystonia: A Historical Perspective
Presenter:
Stephen P. Kraft, MD, FRCSC
– Department of Ophthalmology and Vision Sciences, University of Toronto, Toronto, Ontario, Canada
Contents:
- A Surprising Discovery in the Sistine Chapel
- What Are Dystonias?
- Various Associated Problems
- Where in the brain does this problem arise?
- What is Hemifacial Spasm?
Dr. Kraft began his presentation with a story that illustrates how medical discoveries can happen in unexpected ways. And in fact, his whole presentation turned out to be about those unexpected moments of enlightenment!
Dr. Kraft's Presentation - A Synopsis
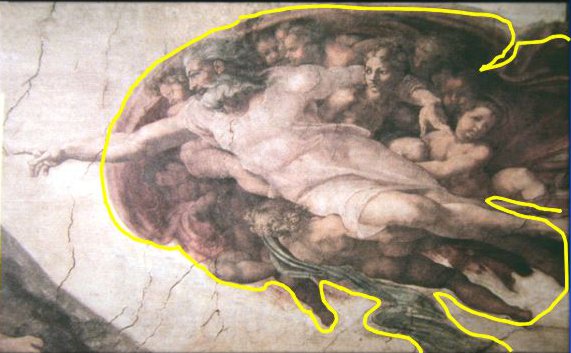
“This slide is one of the panels painted by Michelangelo which is located in the Sistine Chapel. He actually hid some things into these panels, and if you know where to look you’ll find these hidden images. This scene of God creating Adam is one that is very familiar to most of you, but you likely didn’t recognize everything that you were seeing in it!
“Well, if we start to draw a line around the outer border of the picture, you will see something remarkable about that big apparently amorphous mass in the background. It’s actually . . . a brain!

“The story of this initial discovery is very interesting. There was a medical student who did his undergraduate major in art and went to one of the eastern US schools for medical training. And one day, when he was studying his anatomy diagrams, he decided to take a break and go and look at some art. By fluke, he had opened his neurological anatomy book to the page with a diagram of the brain, at the same time he was looking at a picture of this panel of the Sistine Chapel.
“And he looked at it and said 'You know what? The outline of the picture exactly matches the outline and superficial structures of the brain.'

“Michelangelo left no record to explain what hidden images he created in these frescoes, but there are thought to be 20 of the 64 frescoes in the Sistine Chapel that have anatomical body parts hidden in them.
“So, for 400 years the secret of these hidden anatomic images wasn’t picked up, until 1983 when this medical student made this discovery.
“So to the subject of this talk: Slide #4 shows an example of the disease we’re talking about. One of the neurologic diseases that are called dystonias.
“Dystonias are a series of neurologic problems where you can't control the movements of one or more parts of the body. Blepharospasm is the disorder specifically related to muscles around the eyes, and sometimes lower face and neck too, and this is what we are trying to treat.
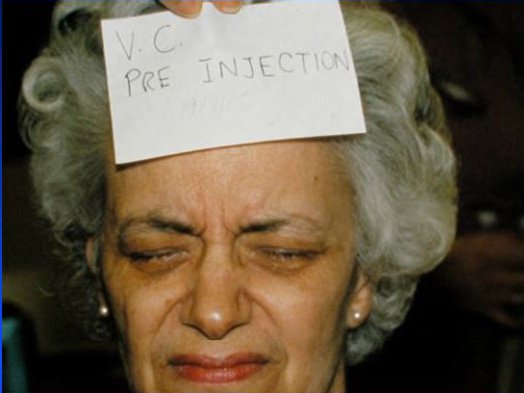
“It usually starts in the middle to late age groups. And it’s reported to be slightly more common in females, and I think that’s probably been my experience over 35 years as well. And you get uncontrolled spasm of the periocular and also facial muscles. And it can spread from the eyelids to other parts of the face.
“It is called Meige syndrome when the spasms spread to involve lower parts of the face. Before Botox, or botulinum toxin, the only treatments were oral medications and eyelid surgery, which some of my patients have gone through over the years.
Benign Essential Blepharospasm
- Onset in 5th-6th decades of life
- Slight female preponderance
- Uncontrolled spasms of the periocular facial muscles
- Can spread to or involve lower facial and/or neck muscles (Meige syndrome)
- Prior to Botox only treatments were oral medications and eyelid surgery
“In the last couple of years some new information was published about dystonias. This is an article from a new journal that looks at diseases as a whole, and goes back and looks at the recent literature and recent developments and gives you kind of a picture of the current state of the art. These two gentlemen in 2016 described how we look at the disease in terms of rating patients’ severity and how we categorize patients’ disease signs.
“Currently there’s a rating severity that uses six criteria; we used to have only two or three. But we now record how long the eyelid closures occur, the frequency, and the presence of apraxia, in addition to how intense they are (still using the scale which is called the Jankovic scale which we have used for many years).
Rating of Severity of Blepharospasm:
- Duration of eye closure episodes
- Degree of intensity of eyelid closure
- Frequency of spasms
- Presence of apraxia
- Presence of spasms during writing tasks
- Increase in blink rate
Frontiers in Neurology, 2016
“Apraxia is a neurologic problem where you can open your eyes but you can't initiate the opening reflex. In other words, your eyes are closed, and when you are asked to open your eyes, the signal to do that is delayed or it doesn’t exist for a while, and you have to actually use tricks to try and get the eyes open. And this is another disorder different from blepharospasm. But some people with blepharospasm also have apraxia. And sometimes the only way we know that is, when you relax the muscles with botulinum, you no longer have the spasms, but you can't physically open the eye even though there’s no spasms keeping them closed anymore. So, your eyes stay closed not because of tension from the spasm, but because you can't initiate the opening motion, and that adds a little bit more complexity to the treatment.
“Also, the presence of spasm during writing tasks is now a criteria for the severity, because it seems that for some people, when they’re writing or doing tasks up close, things are better, whereas for other people it’s worse. So, if you have problems keeping your eyes open during writing or tasks up close, it adds another degree of severity because it affects a common daily activity that people have to be able to do, that is, to read or write.
“Blepharospasm can also increase the blink rate, which many of you have. But it’s mainly the tightness of lid closure, how long it’s acting for, and how long it takes you to open your eyes that are the main criteria that neurologists are using to rate the severity of the disorder.
Associated Symptoms in Cranial Dystonia
- Sensory: eye grittiness, dryness, “burning”
- Psychologic: anxiety, depression
- Sleep disturbances
- Cognitive: reduced working memory & information processing (not assoc’d with BEB)
Frontiers in Neurology, 2016
“And there are various associated problems with dystonia in general. Not everybody has these. And blepharospasm seems to have a lower incidence of these issues, so I don’t want you to get worried that a lot of this is applying to you. But people who have dystonia in several muscle groups do have other tendencies to psychological issues and sleep disturbances — that’s now something we always ask about — and memory and information processing.
“These issues are more common in dystonia, which is a more diffuse medical condition, but not nearly as common with straight blepharospasm.
“So, if you have spasms in the upper face alone it doesn’t seem to be commonly related to memory issues or concentration issues. But they can be associated with sleep disturbances and with eye symptoms like dryness and grittiness.
“So I’d say at least 80% of the patients I see also need artificial tears because it’s very common to have grittiness or sandy feeling in the eyes, probably from the blinking, but it can also be due to actual dryness of the eye. This is very common in folks in the older age groups, even who do not have essential blepharospasm, and many of you are in the same age range. So we don’t know if they’re always associated, but it’s very common and most of my patients end up needing artificial tears.
“Concerning imaging of the brain, people often ask, ‘Well what’s the latest in terms of where in the brain does this problem arise.’ The good news is that we pretty well know where the problem lies.
Imaging of the Brain:
- Showed abnormalities in only 1.6% of 1100 patients with blepharospasm and cranial dystonia
- Wide distribution of network of pathways affected, including thalamus, lower brainstem, basal ganglia, cerebellum, and midbrain
Frontiers in Neurology, 2016
“However, it is very rare to actually see any changes within the brain itself on imaging. In the few patients who have shown abnormalities, the changes can occur in almost every part of the brain (as circled in the diagram), but these are very subtle — no tumors, nothing like multiple sclerosis, not any of the severe neurologic things, but sometimes just small changes in the brain matter or change in the blood vessels. One frustrating issue is that these findings are not consistent among people, and they do not necessarily occur in the same parts of the brain among patients. So there does not seem to be one part of the brain that is abnormal to explain the problems in all people with blepharospasm.
“And if you look, these authors reviewed several years of studies and, among over a thousand patients who have had imaging, look at how rarely they find anything: in only about 2% of blepharospasm patients!
“In the slide I have circled all the areas that have shown abnormalities, but, again, these are found only in up to 2% of people. So the chance is, your neurologist, if they see nothing else other than blepharospasm with no other neurologic symptoms, they are probably not going to send you for a brain scan, because the chance of finding anything is less than 2% and it’s not something that really is going to change the management.
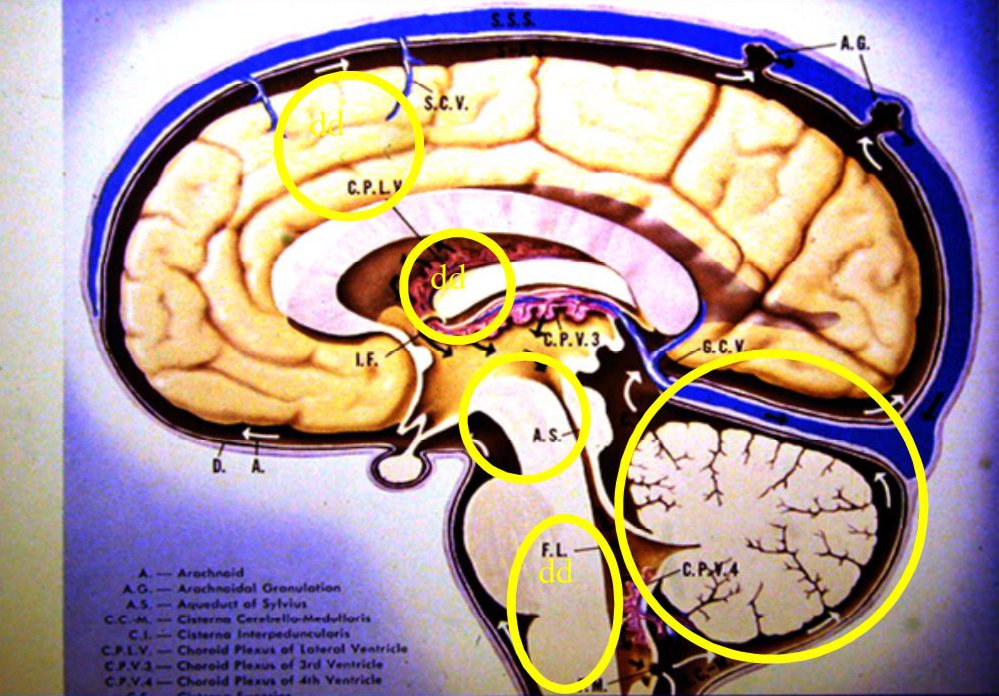
“There are functional MRI studies as well. These are active real-time metabolic studies of the brain and they have show mainly glucose metabolism abnormalities in these same areas as I circled. But what it means no one’s quite sure because we don’t find any benefit from changing sugar intake, and we don’t give you insulin or other interventions that diabetic patients get. So we don’t know exactly what these metabolic studies mean.
“In fact, these areas show extra activity, not lack of activity, in these studies. The excess activity are most commonly where you might expect to find them: in the frontal parts of the brain which control movement, and also in the central parts of the brain which coordinate movement.
“The other thing that’s interesting is that when people are blinking, the parts of the brain dealing with blinking light up more and show more biochemical activity than in normal patients. So again, it just goes along with the fact that your brain is making you blink more, but that doesn’t add new information. We already know that based on your excessive blinking, so it doesn’t tell you any information about what in the brain is the actual abnormality.
Metabolic Studies of the Brain:
- Abnormal glucose metabolism in striatum, thalamus, and in the areas of frontal lobes that have control of eyelid movements
- Exaggerated blink reflex in response to external stimuli, with increase in orbicularis oculi activity
Frontiers in Neurology, 2016
“When we talk about diseases like Parkinson’s or Huntington’s chorea, we know exactly where in the brain those problems are and where the biochemical problem is. In blepharospasm all of those chemicals seem to be functioning normally although in some areas of the brain there’s extra activity. But we don’t know why.
“Before botulinum toxin we used to use oral medications. They were trying to modify certain chemicals in the brain to reduce the extra activity in the brain, but it didn’t work for everybody because, again, there was no way of knowing, from one patient to the next, what part of the brain or what metabolic problem you were dealing with, so it was more of a hit and miss for patients. And that’s why botulinum has become the mode of treatment, because you can directly treat the muscles and not worry what part of the brain may be overworking in the patient.
“That is totally different from this other disease which is called hemifacial spasm.
“Hemifacial spasm is actually not a dystonia. There’s uncontrolled movements on one side of the face but it is not dystonia because it’s got an anatomic physical reason for it. It’s not a biochemical reason. And this can happen in any age group. I’ve had them from the 20s on.
“In fact, my longest treated patient is a young man that I started treating when he was 25, and he’s now 60 something, and he’s been one of my most loyal customers! He’s up to about 90 treatments now and he just keeps coming back, now about once or twice a year. In between treatments he goes on cruises, so he’s happy he’s got his spasms under control.
“We know exactly what the problem is in hemifacial spasm. I have circled a nerve here in this diagram, called the facial nerve. It sends messages that make all the muscles of one side of your face contract. So if you want to move one side of your face – there’s about 22 muscles – there’s one nerve that goes from behind the ear to all these muscles. It’s like your electrical wiring to the neighbourhood. There’s one transformer that sends electrical simulation to the houses on the block. If there is an energy surge, then the lights in all of the houses begin to flicker, and this is the same thing here. There’s one nerve serving all of these muscles. If that nerve is touched, it’s like a “short circuit” in the brain, and all those muscles start firing and cause spasms on one side of the face.
“I have circled the nerve right there, labelled as VII, or 7th. In the next diagram, you can see that there’s a blood vessel, which is an artery, that runs alongside the 7th nerve. And if that artery, instead of going straight, kinks a little bit, it hits that nerve and it’s like setting off an electric discharge, just like in the neighbourhood transformer surge to all the houses.
“We know how to fix that: with neurosurgery. And there are some people in Canada that are really good at it. They used to have to make a large opening to repair it. Now they make a very small opening and they put a little Teflon between the nerve and the artery to stop them from touching. It’s like rewiring in your house where you separate the wires so they don’t short circuit. And that can cure this problem.
“The thing is that a lot of the folks who have hemifacial spasm are in the older age group, and instead of surgery most of them choose to have Botox or Xeomin, which is still a very effective treatment for it. And they don’t mind coming back every 3-4 months for injections. The only problem is that, in contrast to blepharospasm, because you’re treating one side of the face, their wrinkles go away on one side, since those muscles get relaxed. Occasionally some will ask for cosmetic injections on the opposite side to match up the smoothing of wrinkles on the two sides of the face!
“From a historic perspective, prior to the 1980s, to treat blepharospasm, you only really had oral medications, or else what was a fairly drastic eyelid surgery where they removed the muscles in the eyelids and the brow. Currently, in severe cases we sometimes will add a low dose of an oral drug. And, rarely, we still have a last resort of eyelid surgery, done by specialists like our other BEBCRF medical directors, Drs. Khan and Gill. But the lid surgery they do now is much less extensive and complicated than what used to be done.Nowadays the surgery is called a partial myectomy, whereby they take out just enough muscle to get you to stop having spasms but not enough to leave the eye totally open or too sensitive to wind and cold. They do the surgery without creating much damage to your eyelid opening and closing reflexes. But it’s very rare that we do that now, since most patients respond well or reasonably well to eyelid injections.
“I remember when biofeedback was a popular alternative for blepharospasm for a long time. It fell to the wayside for a number of years, but there are people who have gone back to using it. Dr. Farias, whom we've had as a guest lecturer, uses a type of biofeedback to train patients to control their spasms, a treatment that can last a year or longer. But there are few people who go through this procedure.
“For hemifacial spasm, biofeedback was used for a long time. But neurosurgery was still the mainstay of treatment since this is an anatomic problem. Oral medications were less effective than for blepharospasm, but some people did respond to the same drugs used for seizure control, even though hemifacial spasm is not in the same category as epilepsy.
“And then for either disorder there is the good old tried and true approach: prayer. There is a certain remission rate. I can't tell you what it is because I have a lot of patients who have come through my hands that I don’t see anymore. I know some have passed on, but I know many of them have not. And I’m not sure if they’ve just moved or went to someone else for treatment. So I don't know how many of them got better on their own and haven’t comeback because they don’t need the treatments anymore. I have no handle on that. But I’ve had maybe a half dozen patients over my 35 year career who stopped coming for a time,and then came back 10 or 12 years later and said that they were good for a while and the spasm have come back. And now a word or two about botulinum toxin.
“So here again is the trivia question about the original use for which the drug was developed.
“The answer is, it was developed to treat misaligned eyes in adults and children.
“We don’t solicit or support any one formulation. There are four different botulinum drugs made by different companies. The original was developed in San Francisco by eye surgeons who treated crossed eyes in kids and adults, like me. The first human patients were treated under a research study in 1978. So we are now 40 years since the botulinum era began.
“As an example, here’s a photo of a young man who has a crossed right eye. I injected his inner-pulling muscle that was overacting, and now you can see that he’s straight.
“Using this drug for eye muscles is not like the facial spasm or cosmetic treatments, where you have to keep doing it every three or four months. Eyes can actually straighten with one treatment because, in contrast to the facial muscles, the eye muscles are balanced like levers. And if you relax one, the opposite one will naturally tighten. It doesn’t happen in the face; there’s no “balancing” muscle. When you relax the muscle there’s nothing to take up slack to create a lasting improvement. So in the face, once that muscle recovers, you’ve got to inject it again.
“QUESTION: My niece has strabismus She had the operation for it. So why was she given the operation rather than Botox?
“The reason is because the success with surgery is still much higher. And, in kids the turn is usually very large. Botulinum can only straighten it up to about 10° on a lasting basis. If you inject it several times like we do blepharospasm, you might straighten them more and more each time. But the long-term results with large turns is that it’ll keep coming back eventually. So you want a method that’s got the best chance to get them straight long term early in life, before they’re one and a half to two years old. So you want a method that’s got the best chance to get them straight long term early and not fool around with two or three and keep having it recurring, because then their long-term result is not as good.
“Now, when was botulinum first described?
“Believe it or not, we are more than 200 years out from when the medical effects of botulinum were actually known. So this is not a new drug. It’s a new drug, but it’s not a known quantity that’s only recently discovered. Justinus Kerner in Germany actually figured out this disease, and it’s called botulism. And there are outbreaks that happened even in Roman times. Livy and other writers wrote about serious epidemics where people’s muscles faded and they couldn’t breathe and they died. And the thought that it came from contaminated meats goes back hundreds of years.
“And then in 1822 a gentleman by the name of Kerner actually said we should be able to use this as a therapeutic treatment for neurologic diseases! So almost 200 years ago someone actually had an idea that this might be used as a treatment at some point!
“In 1895 was when researchers found out that there are multiple different botulinum strains. Each different bacterium produces a different type of toxin. There are seven different kinds, named A through G, that all have different effects in the body.
“Finally, in the 1940s and ‘50s, came Schantz and Brook. They characterized the A-type of botulinum, which is in Botox, Dysport, and Xeomin. Now Schantz, who lives in Wisconsin, is very famous. He is the expert who provided the original botulinum bacterial strains to Alan Scott in San Francisco so he could create the therapeutic drug. You can see Dr. Scott in this photo from a recent trip my wife and I took to Brazil. He is the one circled in the photo.
“The drug was originally called Oculinum, since it was only used for eye problems. This formulation of botulinum toxin was first approved in Canada in 1983. Dr. Jean Carruthers, a paediatric ophthalmologist in Vancouver, was the first Canadian to use it, and I was the second, actually at the same time as a colleague in Montreal. In the United States it wasn’t approved until six years later. So there was a stage where the FDA hadn’t approved it and American ophthalmologists couldn’t use it, and I had some Americans coming up to Canada to get their injections.
“The first patient that I treated here was at the Toronto General Hospital in January of 1985. Oculinum was still under research protocol. So we got the drug for free and we just charged patients a standard fee to send to Alan Scott to support his research and the licence and shipping costs. And so from 1978 until 1991 you could only get this drug in North America from his research institute in San Francisco.
“After the FDA approved the drug in the early 1990s for use in eye problems and neurologic disorders, over the years the commercial production of the drug was taken over by different companies. There are three companies that provide it in Canada. The three trade names are Botox (Allergan), Xeomin (Merz), and Dysport (Ipsen).
“The classic sites are shown in this diagram, but I vary the pattern a lot in some patients. With regard to actual treatments, we inject in strategic places in the face to relax the most active muscles. I’ve had some patients come to me and talk to me about some doctors who do the same treatment for everybody irrespective of the pattern of spasms. That’s not the way to do it. I think treatments have to be customized. And very few of my patients have exactly the same treatment regimen since I customize it to the most involved parts of the face and determine the concentration based on the severity of the spasms
“The nice thing about Botox, Dysport, or Xeomin is you can inject right where the muscles are in spasm. We have to be careful about the sites, since some people are more prone to get droopy eyelids, while some are more prone to dryness of the eyes. You then have to alter the drug concentration and sites. And it’s a bit of a trial and error for the first year or so, as it sometimes takes two or three rounds of injections to find the right balance between effectiveness and side effects for a patient.
“You have all had this treatment, as in this photo, where we place the fluid just under the skin very carefully, creating little fluid pockets. And the fluid settles out around the injection site.
“This lady had treatment for blepharospasm. You hope to end up with patients opening their eyes like in the photo. Now you notice she’s got kind of orangey-green stuff around her eyes. That’s the fluorescein fluid that we use to make sure their eyes aren’t dry. She came for a post-treatment visit, and I put the drops in and had a look to make sure her corneas weren’t suffering now that she wasn’t blinking forcefully.
“This gentleman in the photo, I really miss him.He died young. You can see his excellent response to injections on the left side of the face for hemifacial spasm.
“Now I make this point that if you inject under the skin pointing the needle in the wrong direction, the percolated fluid will flow under the skin and can head towards the eyelid, leading to a droopy eyelid, as you see in this next photo.
“So I always inject by pointing the needle away from the eyelids. Even then it could still unexpectedly migrate back toward the central eyelid, but hopefully it reduces that risk. Once it is injected, the toxin takes 3 to 5 days to work. Dr. Gill and I did a study, supported by your donations, looking at the average response time for a treatment as well as the effectiveness over many serial treatments. As shown in the slide, the interval of relief seems to reduce slightly in blepharospasm, but not in hemifacial spasm.
“At my last count, there were about 106 uses for botulinum toxin. One of the major benefits is for children with cerebral palsy confined to wheelchairs, and who have very stiff muscles and can't move easily. Doctors now inject botulinum toxin into the big muscles in the back of their legs, and now they have more freedom of movement. Unfortunately, they need such large doses that eventually they usually become immune to the drug and they have to switch to the other drugs.
“It is also being used for stiff muscles for kids and for people after strokes, and for people with orthopedic issues. They’re using it now for scoliosis. You know, for kids who have curvature of their spine, the surgery now is less intense because they can first inject the muscles that are in spasm, to correct the muscle deformity. Then they don’t have to insert as much hardware at surgery to get their spine in line. And they’re also using it for adult spine disorders.
“In the last five years Health Canada has approved botulinum for migraine use. And it’s used because Botox doesn’t just relax muscles, it relaxes nerves. And nerves are what we think stimulate the blood vessels to create migraine headaches in the brain. So if you inject in the muscles in the face where the nerves originate, the drug migrates into the brain and reduces migraine symptoms.
“Some of my happiest patients are actually my migraine patients, because no longer do they have to be on the heavy drugs needed and they’re not disabled for a day at a time or confined to lie in dark rooms. It’s been a major advance. Oral surgeons are using it for TM joint problems. It’s used for sweat control.
“In 1991 we had the first training session for using botulinum toxin, or Oculinum as it was known then. For the first time we trained people outside of the eye specialty. Neurologists, plastic surgeons, dermatologists, ophthalmologists came to the University of Toronto and we ran a training facility. Allergan who had just taken over the licence for the drug, and renamed it Botox, supported the costs of the course. So that day the number of authorized users of the drug in Ontario increased from 3 to about 35 people.
“In 1981 a very perceptive woman by the name of Matty Lou Koster decided to create a national support group for blepharospasm in the United States. The foundation was based in Texas and they started running annual meetings for information and support for patients. They still run a meeting every year.
“In 1991 we had some very perceptive people in Toronto, by the names of Sam and Olga Meister. Sam is still alive. He’s just turned 95 this year and his late wife Olga was a patient of mine. And they set up a similar foundation in Canada. We met at Mount Sinai for the first time, outside of the hospital. And I had a colleague at the time, my dear friend the late Dr. Martin Kazdan, who was the other Toronto specialist that was treating facial dystonias with Botox. He and I met with the Olga and Sam and with Fred and Helen Martin and established the Canadian foundation.
“We’ve had semi-annual meetings for the last 26 years. We started off at Mount Sinai Hospital, but eventually we settled on North York Civic Centre because it was more central for both of our pools of patients.
“There were other support groups. We’ve had groups in Ottawa, Calgary, Vancouver. We’re just in the throes of starting one in Windsor and the Ottawa area as well. There have been other support groups that have come and gone, and hopefully will be re-established.
“At these meetings we talk about new developments. We’ve also had neurologists come in as well as eye surgeons. We talk about websites and we’ve had sessions for physicians and “Ask the Doctor” sessions which are the highlights of every one of the meetings. And our mandate also was fund raising to support these meetings, but also to fund research by anybody in Canada who is interested in doing research to help us understand these diseases.
“Once again, I refer to the project you funded. Dr. Gill gave this talk to all of the ophthalmologists in Toronto at an annual university research meeting. So thanks to you our message has gone out to a wider audience. And again, the conclusions we had from the long-term study was that hemifacial spasm patients get consistent results without much change in the relief interval, but in blepharospasm it seems over many, many years that the interval does slowly go down. And we want to thank the generous support of all you good folks who have funded that work.
“And thanks to all of the members we actually had a large and successful meeting in 2013. I still use the letter opener I received as a speaker’s gift, so that’s why I know the name of the conference was Eye Opener 2013, to celebrate 20 plus years of support and increased awareness.
“And we had a very good turnout of neurologists and ophthalmologists. We also were able to update many of our members and guests who also attended for an afternoon “ask the Doctors” session.
“We had an impressive cast of presenters, including some of the best people in Canada. We had Earl Consky, neurologist; Anthony Kaufmann, a neurosurgeon from Winnipeg , for surgery; Drs Kazdan, Khan and Gill, oculoplastic surgeons; and Dr. Kraft, ophthalmologist, was the Master of Ceremonies.
“So I hope this talk has given you a perspective of where we have come from as a support group and what our mandate has been. And also a review of the historic aspects of these disorders and the current state of diagnosis and treatment.”

